Intrauterine contraception
The terms used to describe the two different forms of Intrauterine Contraception (IUC) have recently changed. A copper intrauterine device (Cu-IUD) is the term used for what is commonly referred to as a ‘copper coil’, and hormonal intrauterine device (LNG-IUD) is now the term used for what was previously referred to as an Intrauterine system (IUS) and commonly known as a ‘hormonal coil’. In the information that follows we are using ‘device’ instead of ‘coil’ to reflect this new guidance.
What happens during a device fitting procedure?
The nurse or doctor will call you through and ask you some questions. This is to check that it is safe to fit the device, and to answer any questions you have. If you haven’t already had a full sexual health screen you will be offered one. We offer all of our patients a blood test for HIV and Syphilis, and a swab for Chlamydia and Gonorrhoea.
The fitting procedure is explained in this short video:
If you have any concerns about your device fitting or if after reading through this information you have further questions about the procedure you can book a telephone appointment with a nurse by ringing 01273 523 388. There are many things we can do to help make the whole process easier for you
Phone line opening times:
| Monday | 9.15am to 4.30pm |
| Tuesday | 9.15am to 4.30pm |
| Wednesday | 12.30pm to 4.30pm |
| Thursday | 9.15am to 4.30pm |
| Friday | 9.15am to 4.30pm |
*Phone lines are closed on Bank Holidays
Things to remember on the day of the procedure
- Eat! You do not need to avoid food before the procedure, and it is best to have had a light meal and a drink 1-2 hours before your appointment, as this can help to reduce the likelihood of feeling unwell after your device is fitted
- Please make a note of the start date of your last period, or where you are in your contraception pack and bring this with you to the appointment
- Please wear “sensible” underwear (big and stretchy!) and bring a sanitary pad to wear afterwards, as often there is some bleeding and/or discharge after the procedure
- If you have or care for small children or babies please arrange for childcare to avoid bringing them to your appointment. We will need you to lie still and relax. This can be hard to do when you are trying to look after children too
- Please allow 1-2 hours for your appointment. Although the procedure does not take long some people can feel faint afterwards and need a little time to recover
- Please be aware that we have health care professionals of all genders who fit the devices and assist with the procedure. An assistant is needed to ensure your safety and to help the person fitting your IUD. We will do our best to accommodate you if you would prefer to have a clinician or assistant of a specific gender, but please be aware that this may not be possible and therefore may delay your procedure.
- We recommend that you avoid driving immediately after your fitting as you may feel some cramping post procedure
- Try to ensure you have no major commitments for the rest of the day as you may feel a little uncomfortable and need to take it easy afterwards. We recommend sweatpants, a box set and lots of your favourite snacks
Is the device fitting painful? What pain relief do you offer?
Everyone has a different experience when having their device fitted, some have very little discomfort, and others can find it painful. We will do our best to support and reassure you. Please remember you are in control of the procedure and you can ask us to stop or pause at any time.
We usually use a numbing spray on the cervix to help reduce any pain. As a result, you may notice some jelly-like discharge from the vagina after the procedure. Occasionally we may also need to use a cervical ‘block’ (anaesthetic injection into the cervix) to anaesthetise the cervix. If we do, this will be discussed with you at your appointment. It is only the cervix that will be numbed, so you will be able to move around as normal immediately afterwards.
We advise you take an anti-inflammatory painkiller such as Ibuprofen 400mg approximately 1 hour before your appointment unless you know that you are unable to take this type of medication. Alternatively, a paracetamol-based pain killer can be used, or whatever you would usually take to manage period cramps. This is to help with discomfort after the procedure.
Our service offers Entonox, also known as ‘Gas and Air’ or ‘Laughing Gas’ for a short-term pain relief and calming of anxiety during a device fitting. The effects of Entonox usually start within a few breaths, and clear from the body within a few minutes once you have stopped using the Entonox, although some people can feel sick and dizzy for a while after using it. Entonox is not suitable for everyone and should not be used if you:
- Have recently had a ‘burst eardrum’
- Are within 48 hours of scuba diving
- Have had a recent head injury
- Have a lung condition called a ‘pneumothorax’
- If you are driving yourself home you should make sure you feel competent to drive and that it is at least 30 minutes since you stopped using the Entonox.
- Entonox can be used in conjunction with numbing gels and sprays and/ or injections. Your pain relief will be discussed on the day to help you decide which form of pain relief is best for you.
Mindful breathing can be very effective as a method of remaining calm during the procedure, and this can help reduce pain. A simple example can be found here:
After the procedure you may need to continue to take over-the-counter pain relief for the next 24 hours to help relieve any cramps. If your pain continues to worsen please contact us on 01273 523 388
When is the best time to have an IUD fitted?
A device can be fitted at any time during your menstrual cycle, but we need to make sure that you are not at risk of pregnancy when you attend for a device fitting. If there is any risk that you might be pregnant, we will have to reschedule your fitting.
You may be offered a copper intrauterine device as emergency contraception. This can be fitted up to 120 hours after unprotected sex, or within 5 days of your expected date of ovulation. If you need emergency contraception please contact us on 01273 523 388
You may book your appointment at any convenient time providing you are using one of the methods of contraception reliably until your fitting:
- The combined pill, patch or vaginal ring
- The progesterone-only pill (mini-pill)
- Depo-Provera injection within 14 weeks of the last injection
- Implant (Nexplanon) within 3 years of its insertion
- A copper or hormonal device prior to its expiry date
- Condoms used consistently and perfectly (used for the whole period of sexual contact, no breakages or slippage)
If you are currently using the diaphragm or natural family planning (including period tracking apps) OR you are having unprotected sex, you have these options depending on what type of device you are having fitted:
- If you have chosen a copper device you may be able to continue to have unprotected sex until your appointment, but this depends on your menstrual cycle and you will need to discuss this with a contraception-trained doctor or nurse first.
- If you are having a hormonal device fitted please abstain from sex from the first day of your period (Day 1) until your appointment (a hormonal device is preferably fitted between Day 1 and Day 7 of your cycle)
- Alternatively, you can arrange a more reliable form of contraception (from the list above) to be used for more than 3 weeks prior to your fitting appointment
If you have just had a baby, are still breastfeeding or not having periods for any other reason, you will need to discuss the best time to fit your IUD with a contraception trained doctor or nurse
Which type of device should I choose?
We offer different types of device at SHAC:
Levonorgestrel intrauterine device (LNG-IUD or ‘hormonal coil’)
Releases a small amount of hormone into the womb, which thins the lining of the uterus to prevent a fertilised egg implanting and thickens the cervical mucus which makes it difficult for sperm to reach an egg. Depending on the type it can last for 3-8 years. The hormonal device can also help relieve symptoms of heavy menstrual bleeding and period pain, as it can thin the womb lining.
For the first few months after fitting, some people experience hormonal side effects (Mood changes, breast tenderness, acne) and a change to their bleeding pattern (usually lighter and less frequent bleeding). These side effects usually settle within a few months, but if you have any concerns we are happy to talk to you about any side effects you are experiencing.
Hormonal devices commonly used in the UK & how long they can be used for contraception if you are under age 45:
- Mirena – 8 years
- Levosert – 8 years
- Benilexa – 8 years
- Kyleena – 5 years
- Jaydess – 3 years
If you are 45 years or older and have any 52mg levonorgestrel hormonal device (Mirena, Levosert and Benilexa) inserted for contraception then this can be used up until age 55 when contraception is no longer required.
If you use a 52mg levonorgestrel hormonal device as part of hormone replacement therapy (HRT) this will need to be changed 5 yearly at your GP.
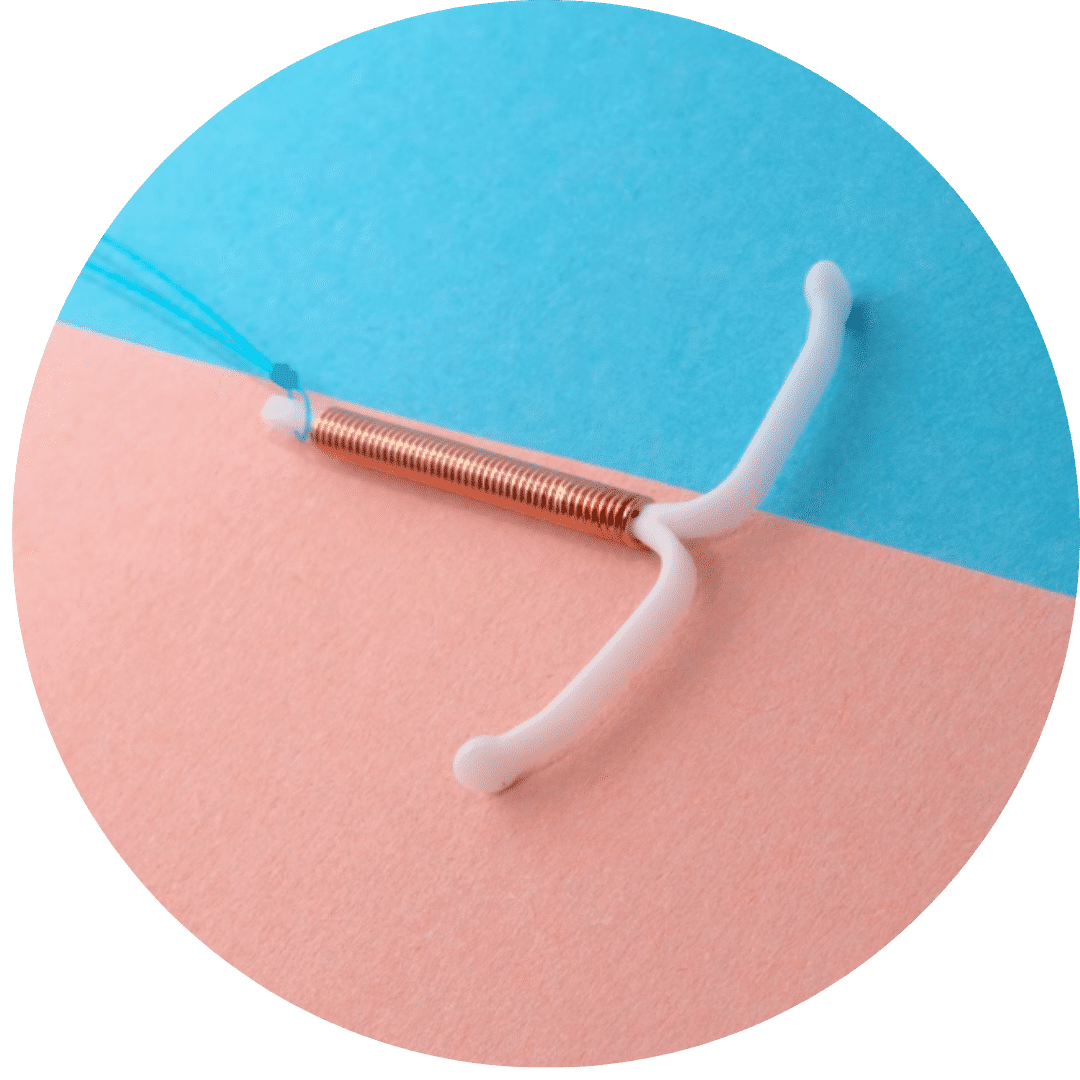
Copper intrauterine device (Cu- IUD or ‘copper coil’)
Has a copper thread woven around the T-shaped device. Copper is toxic to sperm and stops it from reaching an egg and it may also stop a fertilised egg implanting in the uterus. Depending on the type it can last between 5-10 years.
As there are no hormones in a copper device, you will not experience any hormonal side effects. Some people experience heavier menstrual periods with a copper device.
Copper devices used at SHAC and how long they can be used for contraception if you are under age 40:
- Nova-T 380 – 5 years
- T-safe 380A QL – 10 years
If you are 40 years or older any copper device fitted in the UK can be relied on for contraception until age 55 when contraception is no longer required or you have menopause diagnosed if this is sooner.
Both devices can also be fitted at some GP practices in Brighton and Hove.
What are the risks of having a device fitted?
Infection
Although we will do our best to minimise the risk of infection, some people develop an infection after their device fitting procedure. To reduce the risk of this, we advise:
- Having a sexual health screen before the device is fitted, even if you have a regular long-term partner
- Avoid sexual intercourse for the first 4-5 days following in order to let the device settle in and minimise the risk of getting infection
- If you develop any offensive discharge, lower abdominal pain that is worse than period pain, or feel feverish or unwell, please contact us or your GP for advice
Bleeding
Even if the device is not inserted during your period you may have some bleeding for a few days. The local anaesthetic gel used during the procedure may make this look worse.
The device may also cause some unpredictable bleeding over the first 3-6 months after insertion, especially if you have a hormonal IUD fitted. This usually settles down on its own.
If you have prolonged or heavy bleeding (soaking through a sanitary towel every hour) please contact your doctor. If you have had a copper device inserted, heavier periods may be normal.
The use of tampons or moon cups could also disturb the device, so we suggest avoiding using these for 6 weeks following the procedure.
Expulsion
Rarely, the device may come out without you noticing. This is most common in the first three months after fitting. It is a good idea to check you can feel the threads of the device after your period. If you can’t feel the threads, please contact us. You should use extra precautions such as a condom, until a doctor or nurse has checked it is still there.
If your device has come out in the last few days you may need emergency contraception. If it could have come out more than a few days ago, and you are sexually active, we will need to make sure you are not already pregnant before fitting another one or starting alternative contraception.
Damage to the womb
The fitting of a device can, very rarely, become embedded into or perforate (make a small hole in) the womb lining. This happens in less than 2 per 1,000 fittings, often at the time of fitting. It can cause pain, but this is not usually severe and for some people there is no pain. The main symptom is not being able to feel the threads.
If you are unable to feel your threads, please contact us. It may mean that perforation has occurred, but more commonly it means either that the threads are tucked up inside the cervix or (less commonly) the threads have come off the device. If a clinician cannot find your threads, we will carry out an ultrasound scan to check the position of your device. This may require a further appointment. You will be offered another form of contraception until we are sure the device is in the right place.
Ectopic pregnancy
Although your overall risk of becoming pregnant with a device in place is very small (0.2 % with the hormonal device, and 0.6% with a copper device), if you should become pregnant, there is a risk of the embryo developing outside the uterus, usually in one of the fallopian tubes. This is called an ectopic pregnancy and is considered a medical emergency.
If you miss a period (or your period is light and prolonged) and you develop lower, one-sided tummy (abdominal) pain or shoulder-tip pain, please seek urgent medical advice.
Other frequently asked questions (FAQs) about intrauterine device fitting
Can I bring someone with me to my appointment?
You are welcome to bring someone with you for support. We will ask them to wait in the waiting area while we talk to you. This is clinic policy for everyone, and it gives you a space to ask any questions or discuss anything you may want to keep confidential. If you wish, we can then ask them to sit with you during the procedure. However, it is important that they do not obstruct the area the clinician is working in as this increases the risk of infection.
How do I check the threads?
You may be able to feel the threads by inserting two fingers into the vagina and feeling for the threads. If you are concerned that you cannot feel the threads, or see the device come out, we recommend that you use alternate contraception and contact us or your doctor for advice. If you have penetrative sex, your partner should not be able to feel the threads during sex.
What follow-up do I need?
If you are not experiencing any problems with your device there is no need for routine follow-up. However, we will be happy to see you if you are having any issues
How do I get a device removed or replaced?
If you do not wish to continue using your device, you will need to book an appointment for removal. This is usually a straightforward procedure and takes no more than a few minutes. You do not have to wait until your device is expired to have it removed, but we advise that you avoid any penetrative vaginal sex for 1 week before having your device removed, to reduce the risk of an unplanned pregnancy. At your appointment, the clinician will discuss your risk of pregnancy and offer an alternative method of contraception.
If your device is due to expire and you would like another, this can be done in the same appointment.
If you need to replace your current device and it is still in date, then this can be done on any convenient day provided you:
- haven’t had sex for 7 days before the appointment
- use condoms reliably for 7 days before the appointment
This is because occasionally we are unable to fit a new device after removal of the old one resulting in a risk of pregnancy if you have had sex in the previous week. You may be asked to provide a urine sample to exclude a pregnancy on the day of your fit.
What do I need to know if I’m having my device removed for pregnancy?
If you are having your device removed as you plan to get pregnant, we recommend that you begin taking the pre-pregnancy vitamin Folic Acid as soon as possible. This can help prevent problems with the development of the foetus in the very early stages of pregnancy. We also advise that you talk to your GP if you have any medical conditions, or take any medications, so that you can ensure your pregnancy is safely managed to have the healthiest outcome.
Can I exercise after having an IUD fitted?
We advise that you rest on the day of your device fitting, even if you are usually fit and active. This will allow your body to recover. After this there is no restriction to exercise when you have a device.
Can I travel after a device fitting?
It may be a good idea to delay long-distance travel for 6 weeks to make sure you are happy with the method and are not experiencing any difficulties or complications, especially if you are travelling to a location where accessing healthcare may be difficult or expensive!
How soon after a device fitting can I have sex?
Although, depending on the timing, your device may be immediately effective at preventing pregnancy, we recommend you avoid any penetrative vaginal sex for the first 4-5 days to avoid the risk of infection. This includes avoiding any fingers or sex toys inserted into the vagina. Hormonal devices (Mirena, Jaydess, Kyleena and Levosert) may take 7 days to be effective. The clinician that fits your device will explain this to you.
If you experience any pain during sex when you have an intrauterine device, please contact us for advice.